Peut-être avez-vous entendu ce type de réflexion de la part de vos patients atteints de vitiligo. Bien sûr le vitiligo est souvent considéré comme une « simple » affection cutanée mais, pour les personnes concernées, son impact va bien au-delà.
Le vitiligo touche environ 2% de la population mondiale et est la maladie cutanée associée à une dépigmentation de la peau la plus fréquente.2,3 Or, nombreux sont ceux qui minimisent l’impact du vitiligo, pensant qu’il s’agit d’une simple affection cutanée esthétique. En réalité, le vitiligo est une maladie auto-immune de la peau2,3 qui mérite qu’on lui accorde une plus grande priorité en matière de recherche et de traitement.
Adapté de Bibeau, K. et al. Global Valiant Study (2022)
Prévalence du vitiligo dans le monde et en Europe4-9
Prévalence du vitiligo dans le monde et en Europe4-9
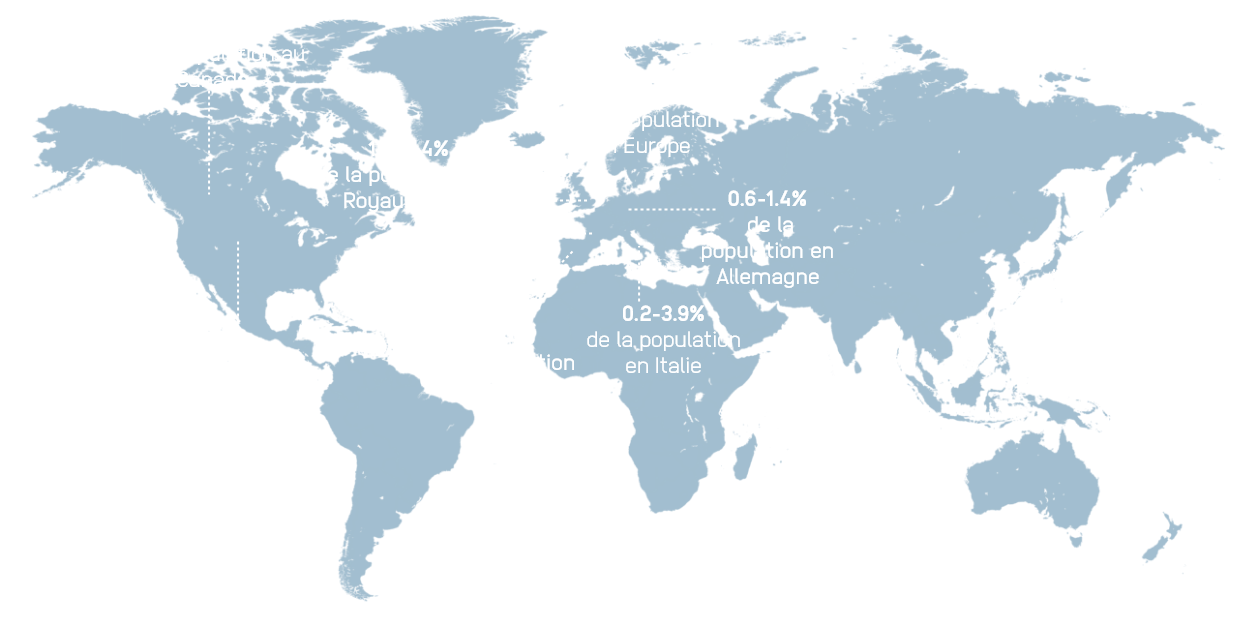
Image adaptée de Krüger C, Schalleuter KU. Int J Dermatol. 2012 ; 51 : 1206-1212, avec la permission de John Wiley and Sons, Copyright 2012 the International Society of Dermatology.

0,1-2,4 % de la population aux États-Unis
2,6% de la population au Canada
1,5-1,8% de la population en Europe
1,3-2,4% de la population au Royaume-Uni
0,3-1,6% de la population en France
0,6-1,4% de la population en Allemagne
1,5-2,4% de la population en Espagne
0.2-3.9% de la population en Italie
0,5-1,7 % de la population au Japon
Image adapted from Krüger C, Schallreuter KU. Int J Dermatol. 2012;51:1206-1212, with permission of John Wiley and Sons, Copyright 2012 the International Society of Dermatology.
- Bibeau K, Hamzavi I, et al. Mental Health and Psychosocial Burden Among Patients Living With Vitiligo: Findings From the Global VALIANT Study. Presented at: Maui Derm for Dermatologists; January 24, 2022; Grand Wailea, Maui, HI.
- Bergqvist C, Ezzedine K. Vitiligo: A Review. Dermatol Basel Switz. 2020;236(6):571-592.
- Bergqvist C, Ezzedine K. Vitiligo: A focus on pathogenesis and its therapeutic implications. J Dermatol. 2021;48(3):252-270.
- Omics online. Omics online vitiligo. Available at: https://www.omicsonline.org/canada/vitiligo-peer-reviewed-pdf-ppt-articles/. Published online 2022. Accessed September 2022.
- Statistics Canada. Table 17-10-0009-01. Population estimates, quarterly. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901. Accessed Sept 2022.
- Harris JE, Ezzedine K, et al. 17755 Global survey investigating the prevalence of vitiligo and vitiligo signs among adults in Europe, Japan, and the United States. J Am Acad Dermatol. 2020;83(6, Supplement):AB198.
- Zhang Y, Cai Y, et al. The Prevalence of Vitiligo: A Meta-Analysis. PLoS One. 2016;11(9):e0163806.
- Bibeau K, Trinidad J, et al. The Prevalence of Vitiligo and Vitiligo Signs in a Broad European Population: Results From the Global Vitiligo Prevalence Study. Published online 2022. Presented at: the European Academy of Dermatology and Venereology Congress; October 9-13, 2019; Madrid, Spain.
- Krüger C, Schallreuter KU. Int J Dermatol. 2012;51:1206-1212.